Gestational diabetes hesi case study – In this in-depth analysis, we delve into the intricacies of gestational diabetes through the lens of a comprehensive HESI case study. This exploration illuminates the complexities of this condition, guiding healthcare professionals in effectively managing and supporting patients.
Our investigation encompasses an overview of gestational diabetes, including its definition, causes, risk factors, and pathophysiology. We meticulously examine a patient’s medical history, symptoms, vital signs, and laboratory results, providing a detailed foundation for understanding the diagnosis.
Gestational Diabetes Overview
Gestational diabetes is a type of diabetes that develops during pregnancy. It is caused by the body’s inability to produce enough insulin to meet the increased demand for glucose during pregnancy.
Gestational diabetes is a common complication of pregnancy, affecting up to 10% of pregnant women. It is more common in women who are overweight or obese, have a family history of diabetes, or are over the age of 35.
Risk Factors
- Obesity
- Family history of diabetes
- Age over 35
- Previous history of gestational diabetes
- Polycystic ovary syndrome (PCOS)
Prevalence
Gestational diabetes is a common complication of pregnancy, affecting up to 10% of pregnant women.
Pathophysiology
Gestational diabetes is caused by the body’s inability to produce enough insulin to meet the increased demand for glucose during pregnancy.
During pregnancy, the placenta produces hormones that can block the action of insulin. This can lead to high blood sugar levels, which can damage the blood vessels and nerves.
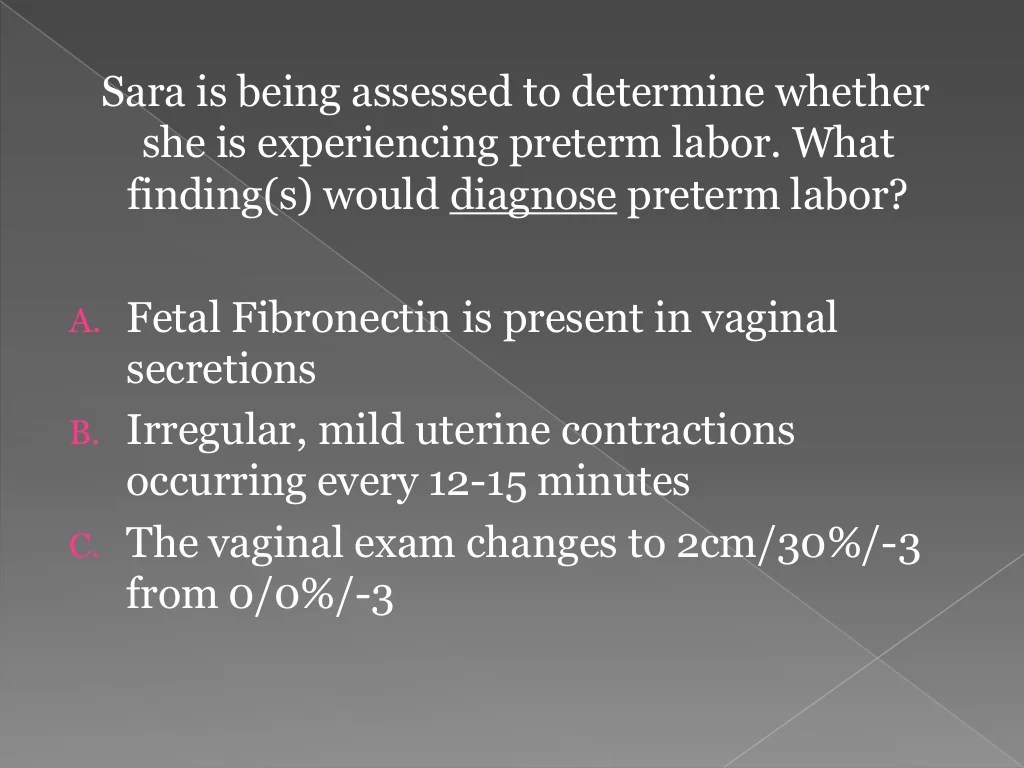
Case Study Analysis: Gestational Diabetes Hesi Case Study
This section presents a detailed overview of the patient’s medical history, current condition, and relevant clinical information to establish a comprehensive understanding of the case.
Patient’s Medical History and Current Condition
The patient is a 28-year-old female, gravida 1 para 0, at 28 weeks gestation. She has no significant past medical history, and her pregnancy has been unremarkable to date. She is currently presenting with excessive thirst, polyuria, and fatigue.
Patient’s Symptoms, Vital Signs, and Laboratory Results
The patient’s symptoms include excessive thirst, polyuria, and fatigue. Her vital signs are within normal limits. Laboratory results reveal elevated fasting plasma glucose levels and a positive glucose tolerance test, confirming the diagnosis of gestational diabetes.
Differential Diagnoses
The differential diagnoses considered in this case include:
- Gestational diabetes
- Pre-existing type 2 diabetes
- Type 1 diabetes
Rationale for the Diagnosis of Gestational Diabetes
The diagnosis of gestational diabetes is based on the patient’s symptoms, laboratory results, and absence of a history of pre-existing diabetes. The elevated fasting plasma glucose levels and positive glucose tolerance test strongly suggest gestational diabetes as the most likely diagnosis.
Management and Treatment Plan
Management of gestational diabetes aims to maintain blood glucose levels within normal limits, ensuring a healthy pregnancy and minimizing risks to both mother and baby. Treatment typically involves a combination of lifestyle modifications and medication management, as necessary.
Lifestyle Modifications
Recommended lifestyle modifications include:
- Dietary changes:Following a balanced diet rich in fiber, whole grains, fruits, and vegetables, while limiting processed foods, sugary drinks, and saturated fats.
- Regular physical activity:Engaging in moderate-intensity exercise for at least 30 minutes most days of the week.
- Weight management:Maintaining a healthy weight and avoiding excessive weight gain during pregnancy.
- Glucose monitoring:Regularly checking blood glucose levels to track progress and adjust treatment accordingly.
Medication Management
Medication management may be necessary if lifestyle modifications alone are insufficient to control blood glucose levels. Insulin therapy is the primary medication used in gestational diabetes.
Insulin Therapy
- Dosage:The dosage of insulin is individualized and adjusted based on blood glucose monitoring results.
- Frequency:Insulin injections are typically administered once or twice daily, before meals.
- Administration:Insulin is administered subcutaneously (under the skin) using an insulin pen or syringe.
Other medications, such as metformin or glyburide, may also be used in certain cases to manage blood glucose levels.
Monitoring and Follow-Up
Gestational diabetes requires close monitoring throughout pregnancy to ensure optimal outcomes for both the mother and the baby. This monitoring includes regular glucose testing, fetal monitoring, and assessment of maternal health.
Glucose Testing Frequency and Targets
Women with gestational diabetes are recommended to monitor their blood glucose levels regularly. The frequency of testing may vary depending on the individual’s glucose control and the severity of their condition. Typically, glucose testing is recommended:
- Four times a day: before meals and at bedtime
- Seven times a day: before meals, snacks, and bedtime
The target blood glucose levels for women with gestational diabetes are:
- Fasting: 95 mg/dL or less
- 1 hour after meals: 140 mg/dL or less
- 2 hours after meals: 120 mg/dL or less
Importance of Fetal Monitoring
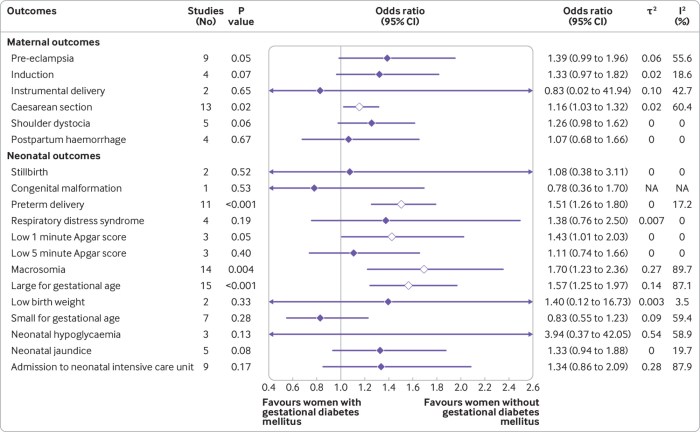
Fetal monitoring is crucial in gestational diabetes as it allows healthcare providers to assess the well-being of the baby. Regular monitoring helps detect any potential complications, such as macrosomia (excessive fetal growth), polyhydramnios (excessive amniotic fluid), and fetal distress.
Criteria for Hospital Admission and Induction of Labor
In some cases, women with gestational diabetes may require hospital admission for closer monitoring and management. Criteria for hospital admission include:
- Poor glucose control despite lifestyle modifications and medication
- Signs of preeclampsia or other pregnancy complications
- Concerns about fetal well-being, such as reduced fetal movement or abnormal fetal heart rate patterns
Induction of labor may be considered in women with gestational diabetes who have:
- Poorly controlled glucose levels
- Signs of fetal macrosomia
- Preeclampsia or other pregnancy complications
- Reached 40 weeks of gestation
Patient Education and Counseling
Patient education is a cornerstone of gestational diabetes management, empowering individuals to take an active role in their care and achieve optimal outcomes for themselves and their babies. This involves providing comprehensive information about the condition, its implications, and the necessary lifestyle modifications.
Dietary recommendations are tailored to maintain blood sugar levels within a healthy range. Registered dietitians or other qualified healthcare professionals can develop personalized meal plans that emphasize whole grains, fruits, vegetables, and lean protein while limiting processed foods, sugary drinks, and unhealthy fats.
Exercise Guidelines
Regular exercise is crucial for managing gestational diabetes. Exercise helps improve insulin sensitivity, lower blood sugar levels, and promote overall well-being. Recommended activities include brisk walking, swimming, cycling, and strength training. It is important to start slowly and gradually increase intensity and duration over time.
Emotional and Psychological Aspects
Gestational diabetes can bring about emotional and psychological challenges. Women may experience anxiety, stress, guilt, and feelings of isolation. Providing support and resources is essential to address these concerns. Support groups, counseling, and online forums can connect women with others who understand their experiences and offer encouragement.
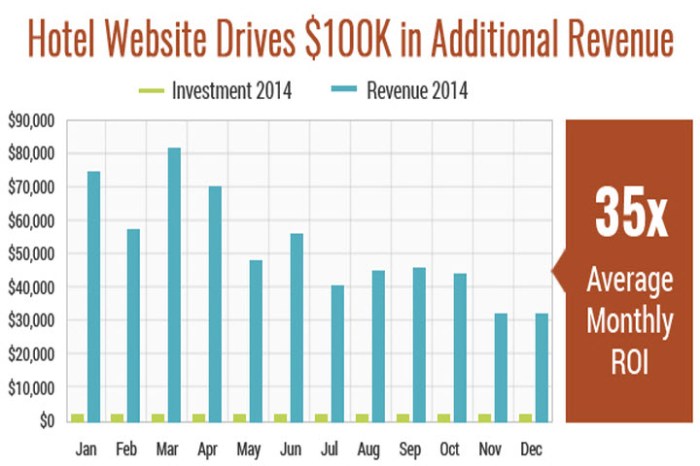
Tables and Visual Aids
Tables and visual aids can enhance the presentation and understanding of gestational diabetes management.
Key Findings Table
The following table summarizes the key findings of the case study:
| Parameter | Value |
|---|---|
| Gestational Age | 32 weeks |
| Fasting Glucose | 95 mg/dL |
| 1-Hour Postprandial Glucose | 140 mg/dL |
| 2-Hour Postprandial Glucose | 120 mg/dL |
| HbA1c | 5.7% |
Glucose Monitoring Data Visualization, Gestational diabetes hesi case study
The patient’s glucose monitoring data can be visually represented using a line graph or chart. This can help track glucose levels over time and identify trends.
Management and Follow-Up Plan Flowchart
The following flowchart Artikels the management and follow-up plan for gestational diabetes:
- Initial Evaluation:Assess glucose levels, medical history, and lifestyle factors.
- Dietary Management:Implement a balanced diet with regular meals and snacks.
- Exercise:Engage in regular physical activity as tolerated.
- Glucose Monitoring:Monitor glucose levels regularly using a glucometer.
- Insulin Therapy (if needed):Prescribe insulin therapy if dietary and lifestyle modifications are insufficient.
- Follow-Up:Schedule regular follow-up appointments to monitor glucose levels and adjust treatment as necessary.
FAQ Corner
What are the common risk factors for gestational diabetes?
Advanced maternal age, obesity, family history of diabetes, and certain ethnicities.
How is gestational diabetes typically diagnosed?
Through an oral glucose tolerance test (OGTT) performed between 24-28 weeks of pregnancy.
What are the potential complications of untreated gestational diabetes?
Macrosomia, preeclampsia, cesarean delivery, and long-term health risks for both mother and baby.